RESEARCH TRIANGLE PARK, N.C. — A new study by health economists at nonprofit research institute RTI International adds to recent research demonstrating a lack of access to affordable mental health and substance use disorder treatment in the U.S.
The study’s findings, detailed in the report Behavioral Health Parity – Pervasive Disparities in Access to In-Network Care Continue, show that patients went out-of-network 3.5 times more often to see a behavioral health clinician than a medical/surgical clinician, 8.9 times more often to see a psychiatrist, 10.6 times more often to see a psychologist, 6.2 times more often for acute behavioral inpatient care, and 19.9 times more often for sub-acute behavioral inpatient care.
The study also revealed that in-network office visit reimbursement, a key lever that health plans use to encourage provider in-network participation, was higher for medical/surgical clinicians than office visits with behavioral clinicians: 22% higher on average; 48% higher at the 75th percentile; and 70% higher at the 95th percentile. Notably, physician assistants were reimbursed for office visits at an average amount 19% higher than psychiatrists and 23% higher than psychologists.
“The finding of large disparities for out-of-network use and reimbursement rates highlights that health plans are not using the same measures to improve the adequacy of their behavioral health provider networks as they do for medical networks,” said lead author Tami L. Mark, PhD, MBA, Distinguished Fellow and director of Behavioral Health Financing and Quality Measurement at RTI. “Our findings echo recent surveys and secret shopper studies that show much greater dissatisfaction with, and lower access to, behavioral health providers than medical/surgical providers.”
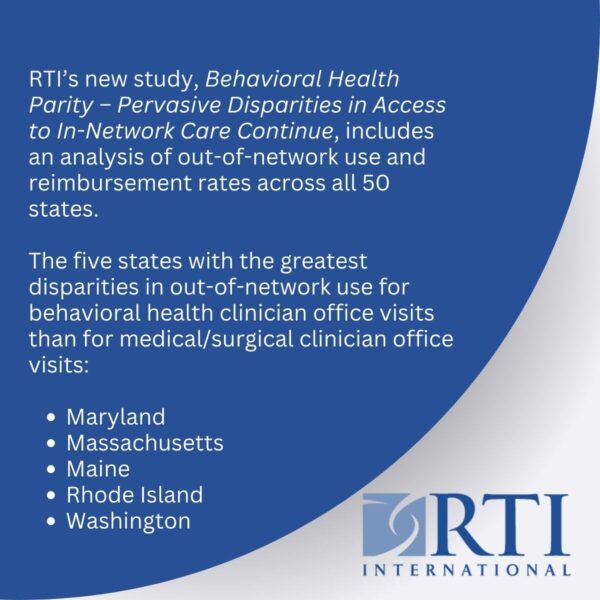
Dr. Mark and co-author William Parish, PhD, used claims and enrollment data from more than 22 million individuals captured annually from 2019 through 2021 to evaluate out-of-network use and reimbursement rates across all 50 states.
“RTI concluded that high out-of-network use for mental health and substance use treatment cannot be explained by a shortage of behavioral health providers,” said Henry Harbin, M.D., senior advisor to The Bowman Family Foundation. “If that were the explanation, we’d see the same out-of-network use disparities for primary care physicians, which are in even shorter supply than mental health providers, according to HRSA, the federal agency that monitors health care workforce shortages.”
The study updates and expands on a previous analysis of parity among privately insured individuals conducted by the actuarial firm Milliman. A comparison between the 2013 and 2021 results reveals no improvement in disparities in out-of-network use.
“Lack of access to affordable and effective care for mental health is at crisis levels in the U.S.,” said Shawn Gremminger, president and CEO of the National Alliance of Healthcare Purchaser Coalitions. “This research demonstrates the profound need for employers and purchasers to demand more of their health insurance carriers to ensure they are providing truly equitable access to behavioral health care in compliance with parity requirements. Employers and purchasers can and must be part of the solution.”
The report was commissioned by the Mental Health Treatment and Research Institute, a tax-exempt subsidiary of The Bowman Family Foundation. A portion of the cost of the report was funded by the American Psychiatric Association, the American Psychological Association, and the National Association for Behavioral Healthcare. The authors are responsible for the content and the views expressed in the report.
Supporters of the report’s recommendations include more than 40 of the nation’s leading mental health and employer groups, many of whom have provided comments about the importance of the research and resulting recommendations, listed here.



